Vitality Tests for Pulp Diagnosis of Traumatized Teeth a Systematic Review

Laser Doppler for Accurate Diagnosis of Oehler's Type Iii Dens Invaginatus: A Case Report
1
Partitioning of Endodontics and Operative Dentistry, Section of Dentistry, Kaohsiung Medical University Hospital, Kaohsiung 807378, Taiwan
2
Division of Periodontics, Department of Dentistry, Kaohsiung Medical University Hospital, Kaohsiung 807378, Taiwan
3
Section of Nuclear Medicine, Due east-DA Hospital, Kaohsiung 824005, Taiwan
four
Partitioning of Orthodontics, Department of Dentistry, Kaohsiung Medical University Hospital, Kaohsiung 807378, Taiwan
5
School of Dentistry, Higher of Dental Medicine, Kaohsiung Medical University, Kaohsiung 807378, Taiwan
half-dozen
School of Dentistry, National Taiwan Academy Medical Higher, Taipei 100225, Taiwan
7
Department of Dentistry, National Taiwan University Hospital, Taipei 100225, Taiwan
8
Division of Oral Pathology & Maxillofacial Radiology, Kaohsiung Medical University Hospital, Kaohsiung 807378, Taiwan
9
Oral & Maxillofacial Imaging Heart, College of Dental Medicine, Kaohsiung Medical University, Kaohsiung 807378, Taiwan
*
Author to whom correspondence should be addressed.
†
These authors contributed as to the 1st author.
Academic Editor: Luca Testarelli
Received: v April 2021 / Revised: 21 April 2021 / Accepted: 22 April 2021 / Published: 24 Apr 2021
Abstract
In vital pulp therapy, pulp testing aids in the differential diagnosis and influences the treatment plan. Different from previous doppler flowmetry studies that only recorded waves and data, we study the kickoff time, the utilise of a laser doppler claret menstruum monitor and imager with a colored epitome to present pulp vitality information in the dental field. We report here a case of Oehlers type IIIa dens invaginatus of the right upper lateral incisor in a 31-year-former girl, with the opening of the invagination near CDJ and a peri-invagination lesion sized 8 × 9 mm2. Cone beam computed tomography was used to verify specific spatial and stereoscopic data. Afterwards removing the source of infection, mineral trioxide amass was selected to fill the invagination. Laser doppler was scheduled for further assessment. Later three years of regular follow-up, the patient'due south clinical condition improved, the peri-invagination lesion healed, and the laser doppler and electrical pulp examination both showed a positive reaction. Laser doppler has successfully improved the diagnostic accuracy Thus, unnecessary interventions tin be avoided while reducing the treatment fourth dimension by preserving the vitality. However, further work is needed to resolve the limitations of laser doppler.
1. Introduction
Dens invaginatus (DI) is a rare dental malformation resulting from an invagination of the tooth crown [1]. In most cases, it occurs when the enamel organ invaginates into the surrounding dental papilla prior to its calcification [2].
The type of endodontic handling and illness prognosis depends on the type of abnormality [iii], and cone beam computed tomography (CBCT) has been used to verify specific spatial and stereoscopic data [four]. Therefore, there is a need for early diagnosis and accurate evaluation of handling options [5,6].
There are diverse concepts, techniques, and materials involved in vital pulp therapy [vii]. Dentists should carefully evaluate the pulp condition and eliminate all infections during the vital pulp handling procedure, which should exist guided past minimally invasive procedures using the optimal cloth and technique to provide the maximum advantages [8].
In vital pulp therapy, dental pulp testing aids the differential diagnosis and influences the treatment plan such as electric lurid testing, propane-butane spray and CO2 [9]. Electric pulp testing, which is commonly used in current clinical practices, functions by stimulating the Aδ fibers in the dentin-pulp complex of the exam tooth through stimulation of a quick, sharp, and transitory tingling sensation [10,11]. Since information technology relies on the patient's subjective feel to respond to the test, the objective cess of the pulp condition is difficult [9,12]. Laser doppler flowmetry (LDF) is a non-invasive, objective, painless test that acquires the frequency-shift signal using optical methods, and subsequently switches to a semi-quantitative style after measurement of the blood period [13]. Light amplification by stimulated emission of radiation doppler has proven to be reliable in previous studies for lurid vitality evaluation and even to assess the healing process of bone lesion of the jaws [fourteen,xv]. This in vivo study demonstrated some of the several advantages laser speckle imaging has over conventional vitality test, making the new instrument more versatile in a clinical environs. However, previous Doppler flowmetry studies but recorded waves and data. Here, we report the get-go time, the employ of light amplification by stimulated emission of radiation doppler blood flow monitor and imager with a colored image to present pulp vitality information in the dental field.
Endodontic treatment of the invagination lonely is advisable for maintaining the vitality of the main root canal pulp [16]. We study here a case of type IIIa DI in the right maxillary lateral incisor with a vital pulp, necrotic invagination, and a large peri-invagination lesion was managed successfully using a conservative approach. Electrical pulp testing and laser doppler claret flow monitor and imager were used in combination to confirm the lurid vitality and provide relevant clinical evidence for the subsequent treatment plan [17].
2. Case Report
A 31-year-old Taiwanese woman underwent orthodontic treatment in the hospital and the routine examination revealed a large peri-invagination lesion with a unique root culvert shape in the upper correct lateral incisor; therefore, she was referred to Endodontics and Operative Dentistry department of Kaohsiung Medical Academy Chung-Ho Memorial Infirmary.
The patient had fair oral hygiene, with no systemic diseases, food or drug allergies, or history of dental trauma. Intraoral examination revealed normal soft tissues with no swelling or sinus tracts. Clinical imaging revealed a peg-shaped clinical crown with no caries or fillings. Notwithstanding, brackets and wires were nowadays in the maxillary teeth with no tenderness or pain on percussion (Figure 1).
The tooth responded normally to thermal and electrical pulp testing (Parkell pulp vitality tester, Farmingdale, NY, Us). Moreover, teeth 11 and thirteen too showed normal responses to both thermal and electric pulp testing. Tooth mobility was grade I. A iv-mm periodontal pocket was detected in the buccal area.
We tin observe the radiolucent invagination from the periapical film (Figure 2a), which looks like a tooth is inside some other. A radiopaque invagination of the dentin lined by the enamel could exist observed in the crown. A "pseudo-canal" was located near the mesial side and extended from the enamel invagination to approximately the cemento-enamel junction, spreading and forming the opening of the pseudo canal, with a lesion at the mesial and lateral role of the root. Considering the irregular shape, root resorption in the "pseudo-culvert" was suspected.
We decided to investigate further with CBCT because of the complex beefcake of tooth 12. Every bit expected, the CBCT scan (EPX-Impla; E-Woo Technology, Yongin, Korea) revealed a blazon III invagination. We can discover from the CBCT coronal view that the pseudo culvert was located nigh the buccal role, while the CBCT sagittal view showed that the buccal side of the pseudo canal with the opening of the invagination well-nigh the cemento-enamel junction, and it was next with a well-defined unilocular peri-invagination radiolucent lesion measuring eight mm (mesiodistal) × 9 mm (labiopalatal) × 12 mm (craniocaudal) (Effigy three). Three-dimensional CBCT aided the diagnosis and provided additional information on the root culvert during the treatment procedure. A diagnosis of Oehler's blazon III DI with necrotic invagination and asymptomatic peri-invagination periodontitis was fabricated. We decided to proceed with the vital pulp therapy of the main canal, followed by nonsurgical endodontic treatment for the pseudo root canal, after discussing the treatment plans with the patient.
Co-ordinate to previous literature [10], the invagination is the usual site of origin of infection. The chief canal is nevertheless vital with no other symptoms; therefore, follow-up was recommended. Regarding the pseudo canal, it was infected, and root culvert therapy was brash. Due to the necrotic invagination, either apexification or revascularization can exist selected. The dentin thickness was sufficient, and it had an open noon on the middle part; therefore, an operation volition not be fourth dimension-consuming. However, the textile should be thick plenty for sealing. MTA, which is more biocompatible, was applied as the filling to the pseudo canal.
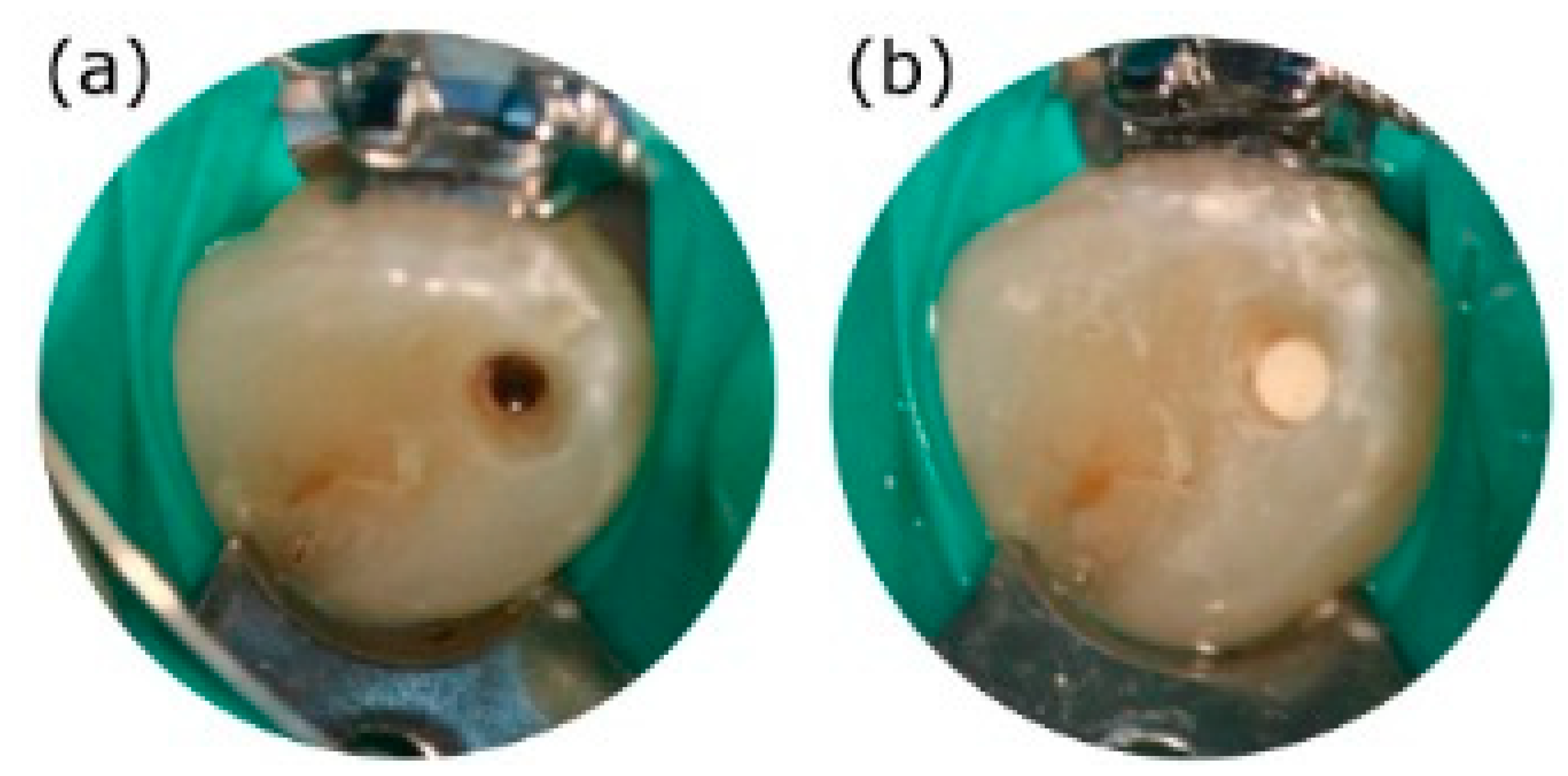
In the first appointment, the access crenel of the invagination was carefully prepared after rubber dam isolation. A surgical operating microscope (OPMI® pico, Carl Zeiss, Oberkochen, Deutschland) was used to prevent damage to the chief canal and for precision. Based on the information from CBCT images regarding the extent, position, and pulpal involvement of the invagination, the pseudo root culvert of tooth 12 was located precisely (Figure 4a).
With the aid of 10-ray imaging and Root ZX mini apex locator (J. Morita Corp., Tokyo, Japan), a 13-mm working length was confirmed (Figure 2b). The pseudo-culvert that appeared to be invaginated was instrumented with Thousand-files upwards to a size lxxx apical master file. During instrumentation, the "pseudo-canal" was immersed in iii% sodium hypochlorite solution and thoroughly rinsed between file changes. After removing the biofilm present on the root canal wall, calcium hydroxide was practical equally the intracanal medication for chemic disinfection. So, the entrance of the operated cavity was covered with 3-mm-thick Cavit (3M ESPE The states, Norristown, PA, U.s.a..) for 12 days.
At the 2nd appointment, the patient returned for a follow-up completely asymptomatic. The temporary restorative materials were removed under rubber dam isolation. Sodium hypochlorite irrigation with a three per centum concentration solution, ISO size 40 stainless steel hand files, and passive ultrasonic irrigation (Obtura Spartan, Algonquin, IL, USA) were used for removing the calcium hydroxide paste. Later on thorough rinsing, a microscopic examination was performed. The corporeality of residual calcium hydroxide was minimized to promote the subsequent mineral trioxide aggregate (MTA) sealing.
At this time, it was recommended that root culvert filling be performed on the pseudo root canal because the infection had been controlled. In improver, follow-up was recommended considering the chief canal was however vital, without whatever symptoms. Furthermore, the pseudo canal was infected. Due to the necrotic invagination with an open up apex, either apexification or revascularization tin be selected, considering the opening on the cemento-enamel junction part of the root canal with a short working length. Notwithstanding, the material should be at least 3-mm, which is thick enough for sealing. Therefore, we chose MTA (Dentsply Tulsa Dental, Tulsa, OK, Us), which is more biocompatible every bit the filling for the invaginated canal (Figure 4b).
A final rinse was performed with normal saline. A sterilized newspaper needle was used to confirm that the "pseudo-canal" was dry out, without exudation of liquid, followed by MTA preparation in accordance with the manufacturer's instructions and recommendations. MTA was practical in layers inside the "pseudo-canal" with proper squeezing and packing. A wet cotton ball was placed inside the root canal to accelerate cloth hardening. Later, the root culvert opening was sealed with Cavit. In the next visit, nosotros restored the tooth with a composite resin (3M ESPE, St. Paul, MN, USA) (Figure 2c). The patient was asymptomatic when she came for followed up half month later.
During the 6-calendar month postoperative follow-up period, the patient did not accept whatsoever clinically significant pain or soft tissue swelling. According to the radiographic examination, the patient had improvements in the lesion and responded to EPT unremarkably. In the deeper portion of the periodontal pocket, a flap surgery was performed by a periodontist to level the root.
However, the orthodontist was concerned that the meaning size of the lesion around the root might affect root move during the orthodontic handling. In add-on, according to the literature, a metal orthodontic gear attached to the molar surface might cause false-positive results in traditional electric pulp testing, thereby leading to an inaccurate evaluation of the pulp vitality. Therefore, laser Doppler claret period monitor and imager (MoorLDI-2λ) was scheduled for further assessment.
In the flux image, red colour indicates the surface area with sufficient supply of blood. In other words, the red parts stand for vital pulp. Therefore, it is suggested that the iii front end teeth are vital. According to the perfusion unit'southward (PU) analysis of the light amplification by stimulated emission of radiation Doppler, circle ane refers to the red circle. Further, the statistics show that PU has no meaning deviation from the other two in the control group. It shows that the tooth is still vital and that regular follow-up could suffice (Effigy 5). Since laser Doppler has successfully enhanced the diagnostic accuracy, unnecessary interventions can be avoided. At two years, the periapical area showed normal bone density (Effigy second). Moreover, the tooth however responded normally to electric pulp testing. The PRICE 2020 flowchart showing the steps involved in the instance report (Figure half dozen).
3. Discussion
In a previous study, the pseudo canal was shown to exist the usual site of origin of infection because the invagination acts equally a region of stagnation for organic substances and provides a conducive surround for microbes [18]. The invagination of the enamel into the dental papilla results in a tunnel lined by dentin and enamel invaginating into the pulp [19].
In this instance report, a necrotic invagination was debrided and filled, and the feasible main root culvert was followed-up [20]. Yet, as other major lesions were nowadays, other dental specialists were consulted. A more accurate lurid diagnosis was required for the treatment plan [21,22].
In 1964, the red blood jail cell velocity evaluation method of collecting frequency-shift signals using optical measurements and switching to a semi-quantitative mode after the measurement of blood flow and volume was first adopted [14,23]. Doppler flowmetry has since been widely used to measure blood menses in soft tissues [24]. Since 1970, laser has been used in diverse clinical fields in Japan and Western countries. In the past decade, with advancements in medical light amplification by stimulated emission of radiation devices, the utilize of lasers in the medical field has become more popular [25]. Laser Doppler mainly uses the Doppler result to notice the lurid claret flow condition [26]. As a diagnostic technique for lurid disease, laser Doppler flowmetry (LDF) improves the accuracy of dental diagnosis, especially for traumatized and permanent teeth [27]. It reduces the diagnostic errors and improves the prognosis of the diseased teeth [9,28].
Laser Doppler is a not-invasive, objective, painless, semi-quantitative method, proven to be reliable and reproducible by numerous studies [29]. Laser is used to discover the pulp blood vessels in which the scarlet blood cells scatter the lite beams and cause Doppler shifts [13,30]. The objective information and imaging scans are presented. The calculated signals in the perfusion units represent the carmine claret jail cell density and velocity to evaluate the pulp vitality after trauma or lurid capping [29,31]. Different from previous Doppler flowmetry studies that only recorded waves and data, we report for the start time, the use of laser Doppler claret flow monitor and imager (MoorLDI-2λ) to evaluate the pulp vitality in the dental field.
As manufacturers have derived various high-end products from the standard models to satisfy applicability for medical research, this study adopted a new-generation light amplification by stimulated emission of radiation Doppler blood flow monitor and imager (MoorLDI-2λ), which allows the observation of authentic images of low claret flow areas in the dental pulp nether the deadening scanning style. It has higher sensitivity, wider dynamic range, and higher resolution compared with previous light amplification by stimulated emission of radiation Doppler flowmetry (LDF). Through laser beam measurement, the mobile interference acquired by traditional operators using the probe is reduced. It does not demand to contact tissues, thus effectively fugitive infections and traumas to tissues. Nonetheless, there are other limitations to the utilise of light amplification by stimulated emission of radiation Doppler imager, such as the cost of the equipment and the interference by inapplicable racket and movement near or in the appliance itself.
Contrary to previous reports, we directly presented the pulp-colored image of the anterior teeth to notice the pulp status in the master root culvert. In combination with the objective information, the perfusion units in the diseased molar did not differ from those in two control teeth, indicating that the master root canal remained feasible. The pulp tissues, rich in claret and lymphatic vessels and nerves, connects to the apportionment through the root apex [32]. They comprise the necessary components of the peripheral immune system and the stalk cells responsible for pulp tissue regeneration. They produce the dentin, maintain dental diet and esthetics, conduct pain awareness, and produce protective responses confronting external stimuli [33]. Maintaining the lurid vitality helps extend the life of the diseased molar. Therefore, before the root culvert therapy, pulp evaluation should exist performed based on the patient's medical history, clinical symptoms, intraoral examination results, and imaging information. When necessary, both light amplification by stimulated emission of radiation Doppler and laser Doppler blood flow monitor and imager tin be used to monitor the pulp claret flow and evaluate the lurid condition to improve the diagnostic accuracy [34], thereby providing relevant clinical evidence for the treatment plan.
4. Conclusions
Although the internal structural complexity of DI makes the root culvert treatment difficult, with the development of minimally invasive procedures, light amplification by stimulated emission of radiation Doppler take successfully enhanced the diagnostic accuracy, accompanied by modern devices and intracanal medication for debridement and a sealing material of good biocompatibility to preserve the healthy pulp tissues. Thus, unnecessary interventions can exist avoided while reducing the treatment time and extending the life of the diseased teeth by preserving the vitality, thereby improving the efficiency and quality of dental care. The factor and movement antiquity noise of the laser Doppler technique motivate ongoing research, and further work is needed to resolve the limitations.
Author Contributions
All authors fabricated substantial contributions to nowadays study. H.-N.L. and F.-H.C. designed the study. H.-Northward.Fifty. and C.-Y.H. analyzed and interpreted the patient data regarding the affliction. S.-C.C. and C.-Y.P. performed the examination of the teeth. J.-H.J. and Y.-K.C. reviewed and editing the original draft training. H.-N.L., D.-Y.Y., and F.-H.C. was a major contributor in writing the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Lath Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Kaohsiung Medical University Hospital (KMUHIRB-E(2)-20180018).
Informed Consent Argument
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Argument
The data presented in this study are available on asking from the respective author within the framework of a scientific cooperation.
Acknowledgments
The authors would like to thank Ying-Chun Lin assistant enquiry fellow of Department of Dentistry, Kaohsiung Medical University Hospital for editing assistance.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Alani, A.; Bishop, K. Dens invaginatus. Part 1: Classification, prevalence and aetiology. Int. Endod. J. 2008, 41, 1123–1136. [Google Scholar] [CrossRef]
- Agrawal, P.K.; Wankhade, J.; Warhadpande, M. A Rare Case of Type 3 Dens Invaginatus in a Mandibular Second Premolar and Its Nonsurgical Endodontic Management past Using Cone-beam Computed Tomography: A Example Report. J. Endod. 2016, 42, 669–672. [Google Scholar] [CrossRef]
- Capar, I.D.; Ertas, H.; Arslan, H.; Tarim Ertas, E. A retrospective comparative report of cone-beam computed tomography versus rendered panoramic images in identifying the presence, types, and characteristics of dens invaginatus in a Turkish population. J. Endod. 2015, 41, 473–478. [Google Scholar] [CrossRef]
- Liu, J.; Que, One thousand.H.; Xiao, Z.H.; Wen, W. Endodontic management of the maxillary first molars with two root canals: A case report and review of the literature. Globe J. Clin. Cases. 2019, 7, 79–88. [Google Scholar] [CrossRef]
- Altuntas, A.; Cinar, C.; Akal, N. Endodontic treatment of immature maxillary lateral incisor with ii canals: Type 3 dens invaginatus. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, e90–e93. [Google Scholar] [CrossRef]
- Brooks, J.Chiliad.; Ribera, M.J. Successful nonsurgical endodontic outcome of a severely afflicted permanent maxillary canine with dens invaginatus Oehlers type 3. J. Endod. 2014, 40, 1702–1707. [Google Scholar] [CrossRef]
- Keles, A.; Cakici, F. Endodontic treatment of a maxillary lateral incisor with vital pulp, periradicular lesion and type Iii dens invaginatus: A case report. Int. Endod. J. 2010, 43, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Kfir, A.; Telishevsky-Strauss, Y.; Leitner, A.; Metzger, Z. The diagnosis and conservative treatment of a circuitous blazon 3 dens invaginatus using cone axle computed tomography (CBCT) and 3D plastic models. Int. Endod. J. 2013, 46, 275–288. [Google Scholar] [CrossRef] [PubMed]
- Ghouth, N.; Duggal, M.Southward.; BaniHani, A.; Nazzal, H. The diagnostic accuracy of laser Doppler flowmetry in assessing pulp blood flow in permanent teeth: A systematic review. Dent. Traumatol. 2018, 34, 311–319. [Google Scholar] [CrossRef]
- Brignardello-Petersen, R. Laser Doppler flowmetry and pulse oximetry seem to have high accuracy in detecting vital and nonvital teeth and perform better than cold, estrus, and electrical pulp testing. J. Am. Dent. Assoc. 2018, 149, e152. [Google Scholar] [CrossRef] [PubMed]
- Civjan, Due south.; Barone, J.J.; Vaccaro, Thou.J. Electric pulp vitality testers. J. Paring. Res. 1973, 52, 120–126. [Google Scholar] [CrossRef]
- Karayilmaz, H.; Kirzioglu, Z. Comparing of the reliability of laser Doppler flowmetry, pulse oximetry and electrical pulp tester in assessing the pulp vitality of human being teeth. J. Oral. Rehabil. 2011, 38, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Olgart, L.; Gazelius, B.; Lindh-Stromberg, U. Laser Doppler flowmetry in assessing vitality in luxated permanent teeth. Int. Endod. J. 1988, 21, 300–306. [Google Scholar] [CrossRef]
- Ahn, S.Y.; Kim, D.; Park, Due south.H. Long-term Prognosis of Pulpal Condition of Traumatized Teeth Exhibiting Contradictory Results between Lurid Sensibility Exam and Ultrasound Doppler Flowmetry: A Retrospective Study. J. Endod. 2018, 44, 395–404. [Google Scholar] [CrossRef]
- Musu, D.; Shemesh, H.; Boccuzzi, M.; Dettori, C.; Cotti, E. Correction to: The effectiveness of ultrasound examination to assess the healing procedure of bone lesions of the jaws: A systematic review. Clin. Oral Investig. 2020, 24, 3739–3747. [Google Scholar] [CrossRef]
- Lee, J.K.; Hwang, J.J.; Kim, H.C. Handling of peri-invagination lesion and vitality preservation in an immature blazon III dens invaginatus: A instance report. BMC Oral Wellness 2020, 20, 29. [Google Scholar] [CrossRef] [PubMed]
- Gazelius, B.; Lindh-Stromberg, U.; Pettersson, H.; Oberg, P.A. Laser Doppler technique—A future diagnostic tool for tooth lurid vitality. Int. Endod. J. 1993, 26, 8–nine. [Google Scholar] [CrossRef] [PubMed]
- Nosrat, A.; Schneider, S.C. Endodontic Management of a Maxillary Lateral Incisor with 4 Root Canals and a Dens Invaginatus Tract. J. Endod. 2015, 41, 1167–1171. [Google Scholar] [CrossRef]
- Teixido, Grand.; Abella, F.; Duran-Sindreu, F.; Moscoso, S.; Roig, M. The use of cone-beam computed tomography in the preservation of pulp vitality in a maxillary canine with type 3 dens invaginatus and an associated periradicular lesion. J. Endod. 2014, forty, 1501–1504. [Google Scholar] [CrossRef] [PubMed]
- Vier-Pelisser, F.V.; Pelisser, A.; Recuero, Fifty.C.; So, M.V.; Borba, Grand.G.; Figueiredo, J.A. Apply of cone beam computed tomography in the diagnosis, planning and follow up of a type III dens invaginatus case. Int. Endod. J. 2012, 45, 198–208. [Google Scholar] [CrossRef]
- Yang, J.; Zhao, Y.; Qin, M.; Ge, L. Pulp revascularization of young dens invaginatus with periapical periodontitis. J. Endod. 2013, 39, 288–292. [Google Scholar] [CrossRef]
- Zoya, A.; Ali, Due south.; Alam, S.; Tewari, R.One thousand.; Mishra, Southward.K.; Kumar, A.; Andrabi, S.M.-U.-N. Double Dens Invaginatus with Multiple Canals in a Maxillary Central Incisor: Retreatment and Managing Complications. J. Endod. 2015, 41, 1927–1932. [Google Scholar] [CrossRef]
- Ersahan, Due south.; Sabuncuoglu, F.A.; Oktay, E.A. The Efficacy of Laser Doppler Flowmetry, Electrical Pulp Test and Cold Test in Diagnosing Revascularization of Extrusively Luxated Immature Maxillary Incisors. Pak. J. Med. Sci. 2018, 34, 787–793. [Google Scholar] [CrossRef]
- Evans, D.; Reid, J.; Strang, R.; Stirrups, D. A comparing of light amplification by stimulated emission of radiation Doppler flowmetry with other methods of assessing the vitality of traumatised anterior teeth. Endod. Dent. Traumatol. 1999, 15, 284–290. [Google Scholar] [CrossRef]
- Firestone, A.R.; Wheatley, A.Chiliad.; Thuer, U.West. Measurement of blood perfusion in the dental pulp with laser Doppler flowmetry. Int. J. Microcirc. Clin. Exp. 1997, 17, 298–304. [Google Scholar] [CrossRef]
- Gazelius, B.; Olgart, L.; Edwall, B. Restored vitality in luxated teeth assessed by laser Doppler flowmeter. Endod. Dent. Traumatol. 1988, four, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Liao, Q.; Ye, W.; Yue, J.; Zhao, X.; Zhang, L.; Zhang, 50.; Huang, D.; Zheng, Q. Self-repaired Process of a Traumatized Maxillary Central Incisor with Pulp Infarct after Horizontal Root Fracture Monitored by Light amplification by stimulated emission of radiation Doppler Flowmetry Combined with Tissue Oxygen Monitor. J. Endod. 2017, 43, 1218–1222. [Google Scholar] [CrossRef]
- Ingolfsson, A.R.; Tronstad, Fifty.; Hersh, E.V.; Riva, C.E. Efficacy of laser Doppler flowmetry in determining pulp vitality of homo teeth. Endod. Paring. Traumatol. 1994, x, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Ingolfsson, A.Eastward.; Tronstad, L.; Riva, C.E. Reliability of laser Doppler flowmetry in testing vitality of human teeth. Endod. Dent. Traumatol. 1994, 10, 185–187. [Google Scholar] [CrossRef]
- Roy, E.; Alliot-Licht, B.; Dajean-Trutaud, S.; Fraysse, C.; Jean, A.; Armengol, Five. Evaluation of the ability of laser Doppler flowmetry for the assessment of lurid vitality in general dental practice. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Park, S.H. Furnishings of age, sex, and blood pressure level on the blood flow velocity in dental pulp measured by Doppler ultrasound technique. Microcirculation 2016, 23, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Raab, W.H.; Reithmayer, K.; Grund, P. Vitality tests of the molar lurid using laser Doppler flowmetry. Dtsch. Zahnarztl. Z. 1990, 45, 725–727. [Google Scholar] [PubMed]
- Musselwhite, J.Chiliad.; Klitzman, B.; Maixner, Westward.; Burkes, E.J.J. Laser Doppler flowmetry: A clinical test of pulpal vitality. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997, 84, 411–419. [Google Scholar] [CrossRef]
- Winzap-Kalin, C.; Chappuis, 5.; von Arx, T. Laser Doppler flowmetry for vitality testing of traumatized maxillary incisors. Schweiz. Monatsschr. Zahnmed. 2005, 115, 12–17. [Google Scholar] [PubMed]
Figure 1. Clinical test. (a) Intraoral test of a 31-twelvemonth-sometime woman showing normal soft tissue. (b) Incisal view of molar 12 showing a Peg-shaped clinical crown.
Figure ane. Clinical test. (a) Intraoral examination of a 31-year-quondam woman showing normal soft tissue. (b) Incisal view of tooth 12 showing a Peg-shaped clinical crown.
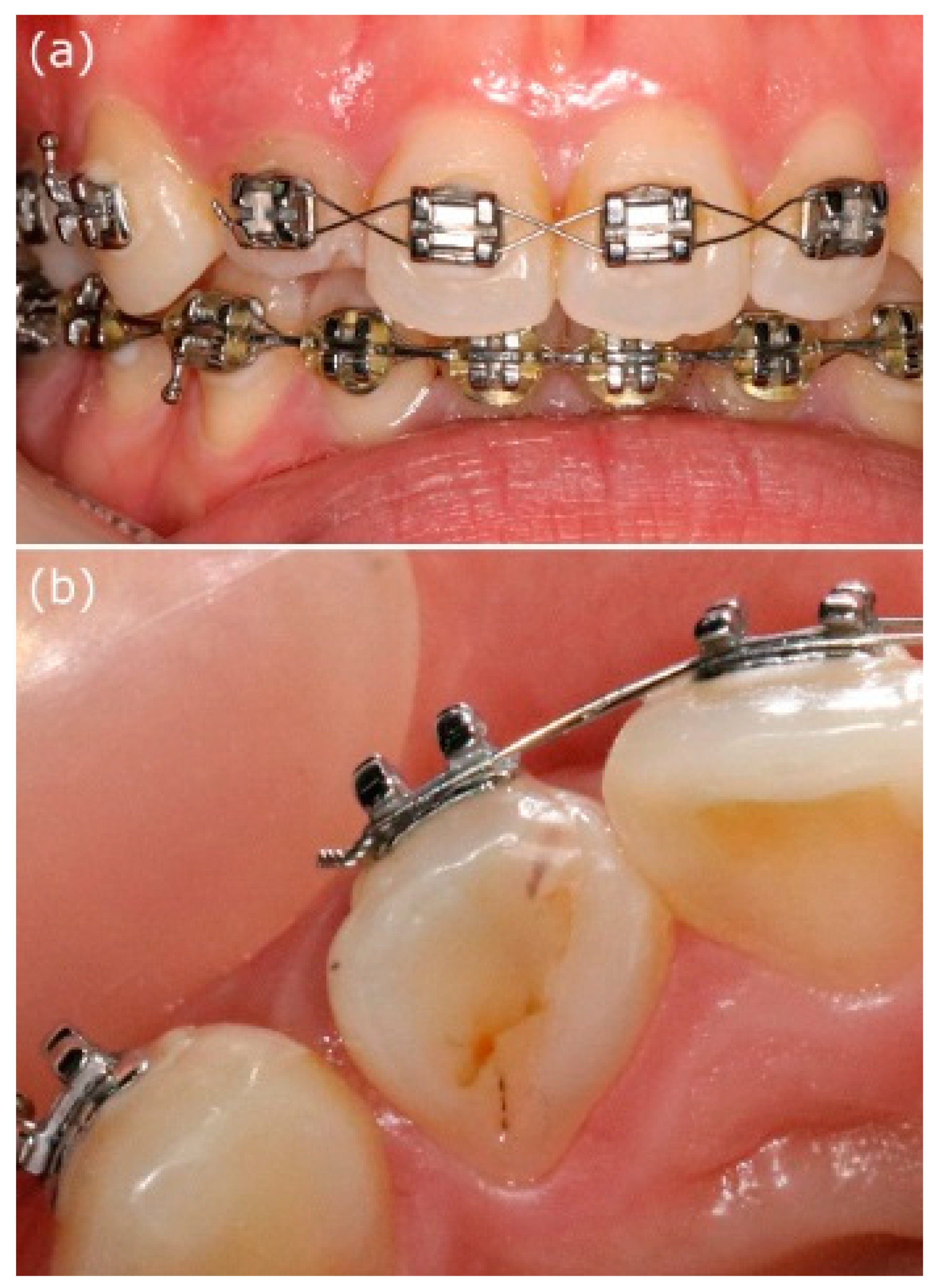
Figure 2. Periapical films during the treatment procedure. (a) X-ray showed that the radiolucent invagination looks like a molar inside another. Additionally, there was dentin invagination lined by enamel into the main canal space, spreading into the mesial function of the middle root. Tooth 12 appeared to be associated with a large peri-invagination radiolucent lesion around the opening of the invagination near CDJ. (b) Measurement of the working length. (c) Mineral trioxide amass was used to seal the invagination. (d) Follow-up at two postoperative years. The patient complained of no clinical symptoms, and the peri-invagination lesion had healed significantly.
Figure 2. Periapical films during the treatment procedure. (a) Ten-ray showed that the radiolucent invagination looks similar a tooth inside another. Additionally, there was dentin invagination lined by enamel into the main canal infinite, spreading into the mesial function of the middle root. Tooth 12 appeared to be associated with a large peri-invagination radiolucent lesion around the opening of the invagination near CDJ. (b) Measurement of the working length. (c) Mineral trioxide aggregate was used to seal the invagination. (d) Follow-upwardly at ii postoperative years. The patient complained of no clinical symptoms, and the peri-invagination lesion had healed significantly.

Figure 3. Different sections in cone-beam computed tomography. (a) From the axial view, "pseudo-canal" can be observed on the mesial side, surrounded by the enamel. (b) The opening of the invagination near CDJ tin be seen in the "pseudo-canal", in the middle-third of the root. (c) From the CBCT coronal view, we tin detect that the pseudo culvert was located virtually the core part. (d) The CBCT sagittal view showing that the buccal side of the pseudo canal with the opening of the invagination near the cemento-enamel junction, and it was next with a well-divers unilocular peri-invagination radiolucent lesion with a size of 8 mm × 9 mm × 12 mm.
Figure 3. Different sections in cone-beam computed tomography. (a) From the axial view, "pseudo-canal" tin can exist observed on the mesial side, surrounded by the enamel. (b) The opening of the invagination virtually CDJ tin can exist seen in the "pseudo-culvert", in the heart-third of the root. (c) From the CBCT coronal view, we tin notice that the pseudo culvert was located near the core part. (d) The CBCT sagittal view showing that the buccal side of the pseudo canal with the opening of the invagination nigh the cemento-enamel junction, and it was side by side with a well-defined unilocular peri-invagination radiolucent lesion with a size of 8 mm × nine mm × 12 mm.
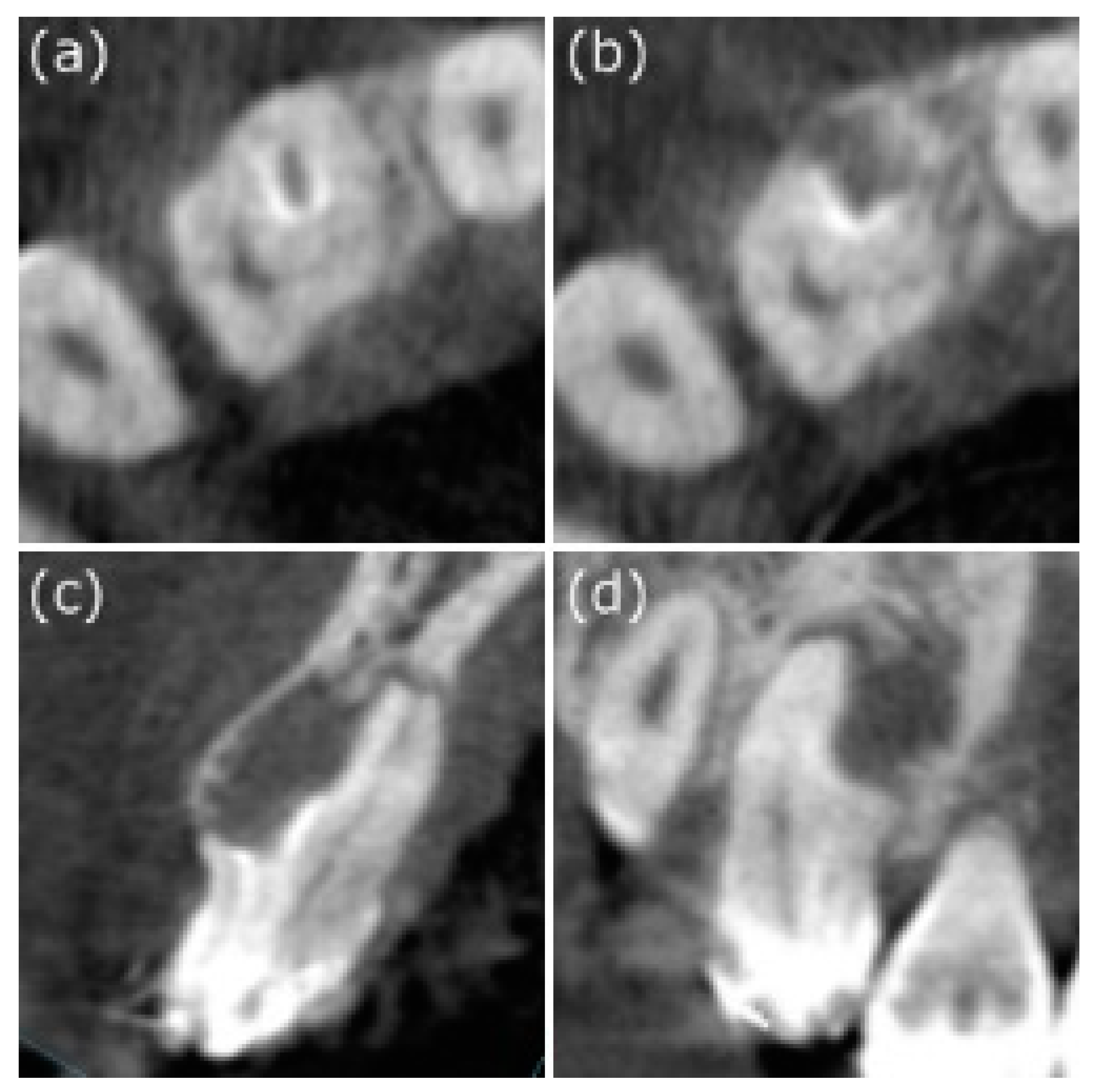
Figure four. Microscopic photos during the handling procedure. (a) The "pseudo-canal" was accurately located under the microscope at a magnification of X9.6 to avert excessive dental tissue loss. (b) Dense mineral trioxide aggregate was filled-in after thorough debridement.
Figure 4. Microscopic photos during the treatment procedure. (a) The "pseudo-culvert" was accurately located under the microscope at a magnification of X9.half dozen to avoid excessive dental tissue loss. (b) Dense mineral trioxide aggregate was filled-in after thorough debridement.
Effigy v. Laser Doppler to track the lurid vitality. (a) In the flux paradigm, the ruby-red color represents areas of abundant blood flow, corresponding to the video epitome (b), in which the carmine circumvolve shows the tooth to be measured. According to (c), PU analysis of laser Doppler revealed that circle ane was the red circle (* means the circle 1 was selected as the reference). The calculated perfusion units in the diseased molar were not significantly different from those in the two control teeth, indicating that the molar remained viable. Continuous follow-upward was recommended.
Figure 5. Laser Doppler to rail the lurid vitality. (a) In the flux prototype, the cherry-red color represents areas of abundant blood flow, corresponding to the video image (b), in which the ruddy circumvolve shows the tooth to be measured. According to (c), PU assay of laser Doppler revealed that circle ane was the red circle (* ways the circle one was selected as the reference). The calculated perfusion units in the diseased molar were not significantly different from those in the ii control teeth, indicating that the molar remained viable. Continuous follow-up was recommended.

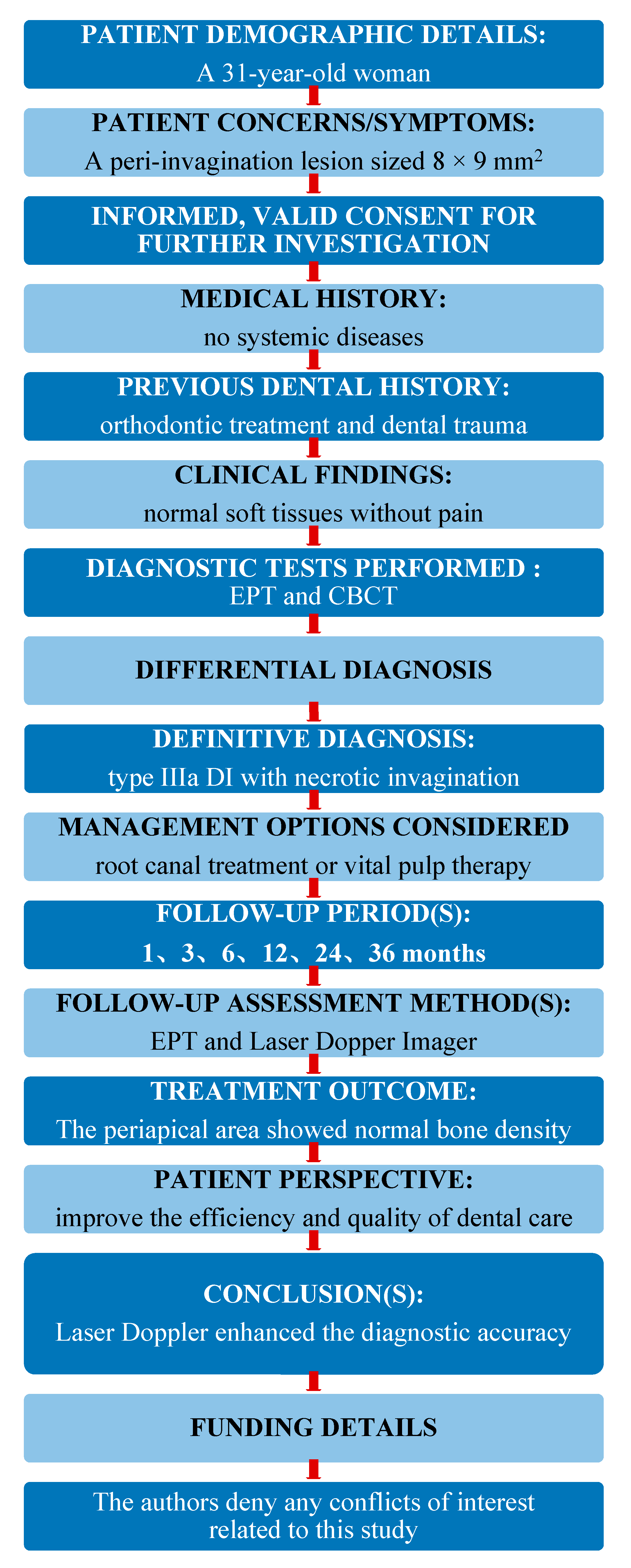
Effigy 6. The Price 2020 flowchart showing the steps involved in the instance report. From: Nagendrababu 5, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PMH (2020) PRICE 2020 Guidelines for reporting instance reports in Endodontics: A consensus-based development. International Endodontic Periodical doi: 10.1111/iej.13285. For further details visit: http://pride-endodonticguidelines.org/price/, accessed on 22 April 2021.
Figure 6. The Cost 2020 flowchart showing the steps involved in the case report. From: Nagendrababu V, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PMH (2020) PRICE 2020 Guidelines for reporting case reports in Endodontics: A consensus-based development. International Endodontic Journal doi: 10.1111/iej.13285. For farther details visit: http://pride-endodonticguidelines.org/price/, accessed on 22 April 2021.
| Publisher'southward Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open up access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/four.0/).
amundsonnotle1941.blogspot.com
Source: https://www.mdpi.com/2076-3417/11/9/3848/htm
 and
and
0 Response to "Vitality Tests for Pulp Diagnosis of Traumatized Teeth a Systematic Review"
Post a Comment